Border Report Section 4 – HIV Diagnoses and People Living with HIV
In 2017, the Texas-Mexico border region had a lower rate of new HIV diagnoses and people living with HIV (PLWH) compared to the rest of Texas. Counties in the Texas-Mexico border region with rates of new HIV diagnoses or PLWH greater than the average for the Texas-Mexico border region are shown in Table 4. The relatively higher rate of PLWH and new HIV diagnoses in Willacy county may be explained by the presence of large (≥3,000 capacity) private correctional facilities located in this county.
Table 4: New HIV Diagnoses and PLWH among Adults/adolescents, 2017, by EMA/TGA and Select Counties from the Texas-Mexico Border Region
| Region |
New HIV |
People Living |
||
|---|---|---|---|---|
|
Number |
Rate* |
Number |
Rate* |
|
|
Texas |
4,391 |
15.5 |
90,700 |
320.4 |
|
Austin TGA |
288 |
13.6 |
6,217 |
293.8 |
|
Dallas EMA |
999 |
20.0 |
22,079 |
442.3 |
|
Fort Worth TGA |
301 |
12.5 |
6,086 |
252.2 |
|
Houston EMA |
1,234 |
20.0 |
28,225 |
457.8 |
|
San Antonio TGA |
382 |
16.5 |
6,674 |
289.1 |
|
East Texas TGA |
310 |
11.3 |
5,864 |
213.6 |
|
All Other Texas |
402 |
8.4 |
6,399 |
133.9 |
|
Texas-Mexico Border |
321 |
11.5 |
5,120 |
184.0 |
|
Border counties with New HIV diagnosis rates above the Texas-Mexico Border average† |
||||
|
El Paso |
124 |
14.8 |
2,179 |
259.3 |
|
Hudspeth |
1 |
22.7^ |
3 |
68.1^ |
|
Presidio |
1 |
14.0^ |
8 |
111.8 |
|
Willacy |
3 |
13.9^ |
37 |
171.4 |
|
Zapata |
2 |
14.0^ |
13 |
90.8 |
* Rates are per 100,000 persons
† Counties not shown had rates of new diagnoses and PLWH at or below the average for the Texas-Mexico border region as a whole.
^ Rates calculated with numerators of 5 or less are statistically unstable and should be interpreted with caution.
Source: Texas eHARS as of July 13, 2018
The epidemiology of new HIV diagnoses in the Texas-Mexico border region is like that of the state overall. A higher percentage of new diagnoses are attributable to men who have sex with men (MSM) transmission (Tables 5a and 5b).
The Texas-Mexico border region has proportionally fewer PLWH compared to other areas of the state. A much higher percentage of PLWH and new HIV diagnoses in the Texas-Mexico border region identify as Hispanic and a lower percentage are female.
Table 5a: Count and Rate of New HIV Diagnoses in the Texas-Mexico Border Region and Texas by Birth Sex, Gender Identity, Race, Age Group, and Mode of Exposure, 2017
|
New HIV Diagnoses |
Texas-Mexico Border Region |
Texas |
||||
|---|---|---|---|---|---|---|
|
Count |
Percent1 |
Rate* |
Count |
Percent1 |
Rate* |
|
|
Total |
321 |
100% |
11.5 |
4,391 |
100% |
15.5 |
|
Birth Sex |
||||||
|
Female |
38 |
12% |
2.7 |
3,758 |
81% |
25.4 |
|
Gender Identity |
||||||
|
Transgender Women |
0 |
- |
- |
59 |
1% |
- |
|
Transgender Men |
0 |
- |
- |
1 |
<1% |
- |
|
Race |
||||||
|
White |
17 |
5% |
6.8 |
845 |
19% |
7.1 |
|
Black |
9 |
3% |
25.3 |
1,621 |
37% |
48.1 |
|
Hispanic |
293 |
91% |
12.0 |
1,758 |
40% |
15.8 |
|
Other |
2 |
<1% |
6.4 |
70 |
2% |
4.7 |
|
Multi-race |
0 |
- |
- |
97 |
2% |
23.6 |
|
Age Group |
||||||
|
0-14 |
0 |
- |
- |
9 |
<1% |
0.1 |
|
15-24 |
63 |
20% |
14.0 |
980 |
22% |
24.5 |
|
25-34 |
117 |
36% |
30.7 |
1,640 |
37% |
39.4 |
|
35-44 |
63 |
20% |
18.1 |
849 |
19% |
22.3 |
|
45-54 |
53 |
17% |
17.0 |
576 |
13% |
16.2 |
|
55-64 |
16 |
5% |
6.1 |
280 |
6% |
8.8 |
|
65+ |
9 |
3% |
2.7 |
57 |
1% |
1.6 |
|
Mode of Exposure |
||||||
|
MSM† |
249 |
78% |
* |
3,126 |
71% |
* |
|
MSM/PWID |
14 |
4% |
* |
135 |
3% |
* |
|
PWID† |
15 |
5% |
* |
228 |
5% |
* |
|
Heterosexual^ |
44 |
14% |
* |
892 |
20% |
* |
|
Perinatal |
0 |
- |
* |
9 |
<1% |
* |
|
Adult Other |
0 |
- |
* |
0 |
0% |
* |
1 Totals are estimated via a CDC-algorithm that determines primary mode of exposure using decimal points. These totals may not add up as rounding to the ones decimal place was implemented.
* Rates are per 100,000 people. Rates calculated with numerators of 5 of less are statistically unstable; interpret with caution
† Persons Who Inject Drugs (PWID), Men who have Sex with Men (MSM)
^ Heterosexual means women who have sex with men and men who have sex with women
Source: Texas eHARS as of July 13, 2018
Table 5b: Count and Rate of People Living with HIV in the Texas-Mexico Border Region and Texas by Birth Sex, Gender Identity, Race, Age Group, and Mode of Exposure, 2017
|
People Living with HIV |
Texas-Mexico Border Region |
Texas |
||||
|---|---|---|---|---|---|---|
|
Count |
Percent1 |
Rate* |
Count |
Percent1 |
Rate* |
|
|
Total |
5,120 |
100% |
184.0 |
90,700 |
100% |
320.4 |
|
Birth Sex |
||||||
|
Female |
831 |
16% |
59.0 |
19,168 |
21% |
136.3 |
|
Male |
4,268 |
83% |
310.7 |
70,832 |
78% |
497.3 |
|
Current Gender Identity |
||||||
|
Transgender Women |
21 |
<1% |
- |
683 |
<1% |
- |
|
Transgender Men |
0 |
- |
- |
17 |
<1% |
- |
|
Race |
||||||
|
White |
344 |
7% |
137.2 |
23,200 |
26% |
195.2 |
|
Black |
144 |
3% |
404.5 |
33,880 |
37% |
1,005.8 |
|
Hispanic |
4,585 |
90% |
186.8 |
29,469 |
32% |
264.1 |
|
Other |
15 |
<1% |
48.1 |
1,060 |
1% |
71.5 |
|
Multi-race |
32 |
<1% |
295.5 |
3,091 |
3% |
752.2 |
|
Age Group |
||||||
|
0-14 |
11 |
<1% |
1.6 |
229 |
<1% |
3.7 |
|
15-24 |
206 |
4% |
46.0 |
3,872 |
4% |
96.9 |
|
25-34 |
978 |
19% |
256.4 |
17,986 |
20% |
432.1 |
|
35-44 |
1,149 |
22% |
330.3 |
20,751 |
23% |
545.4 |
|
45-54 |
1,440 |
28% |
463.2 |
25,412 |
28% |
716.6 |
|
55-64 |
971 |
19% |
372.0 |
17,187 |
19% |
539.6 |
|
65+ |
365 |
7% |
110.7 |
5,263 |
6% |
151.5 |
|
Mode of Exposure |
||||||
|
MSM† |
3,346 |
65% |
* |
55,188 |
61% |
* |
|
MSM/PWID |
203 |
4% |
* |
4,556 |
5% |
* |
|
PWID† |
372 |
7% |
* |
8,724 |
10% |
* |
|
Heterosexual^ |
1,149 |
22% |
* |
21,237 |
23% |
* |
|
Perinatal |
35 |
1% |
* |
856 |
1% |
* |
|
Adult Other |
15 |
<1% |
* |
144 |
<1% |
* |
1 Totals are estimated via a CDC-algorithm that determines primary mode of exposure using decimal points. These totals may not add up as rounding to the ones decimal place was implemented.
* Rates are per 100,000 people. Rates calculated with numerators of 5 of less are statistically unstable; interpret with caution
† Persons Who Inject Drugs (PWID), Men who have Sex with Men (MSM)
^ Heterosexual means women who have sex with men and men who have sex with women
Source: Texas eHARS as of July 13, 2018
A slightly higher percentage of persons diagnosed with HIV in the Texas-Mexico border region received an AIDS diagnosis within three months of their HIV diagnosis. This indicates that their HIV infection was diagnosed late. Potential causes of late diagnosis include decreased access to testing facilities and to general medical care, which may be associated with poverty and lack of health insurance. Receiving a late diagnosis limits the opportunity for early effective treatment and the positive health outcomes that result from early treatment. Encouragingly, there was an 11 percent decrease in late diagnoses along the Texas-Mexico border between 2014 and 2017, which might be a result of increased testing facilities and improved general medical care.
A higher percentage of persons in the Texas-Mexico border Region who were diagnosed with HIV between 2000 and 2017 have survived compared to all Texans diagnosed with HIV in this period. This difference was not as great for persons diagnosed between 1980 and 1999.
Table 6: Late Diagnoses, Death Rates due to HIV and Average Survival in Months
| Outcome |
Texas-Mexico |
Texas |
|---|---|---|
|
Late Diagnoses (AIDS diagnosis ≤ 3 months after HIV diagnosis) as a percent of HIV diagnoses in 2016 |
28% |
27% |
|
Death Rate (per 100,000 PLWH) due to HIV (2015) |
1.7 |
2.6 |
|
Percent of HIV Cases Surviving as of December 31, 2017, by year of diagnosis |
||
|
1980-1989 |
1% |
2% |
|
1990-1999 |
16% |
16% |
|
2000-2009 |
36% |
34% |
|
2010-2017 |
38% |
35% |
Source: Texas eHARS as of July 13, 2018
Gardner’s HIV Treatment Cascade is a graphic tool used to demonstrate whether people living with HIV are receiving recommended clinical care and achieving outcomes that will keep them healthy. Achieving viral suppression is vital for prolonging and improving the quality of life among PLWH and reducing the risk of transmission to their partners. PLWH in the Texas-Mexico border region have slightly lower indicators of met need and retention in care when compared to the state as a whole. However, it is noteworthy that a slightly higher percentage of PLWH in the Texas-Mexico border region achieved viral suppression.
Figure 5. Gardner’s HIV Treatment Cascade for Texas and the Texas-Mexico Border Region, 2017
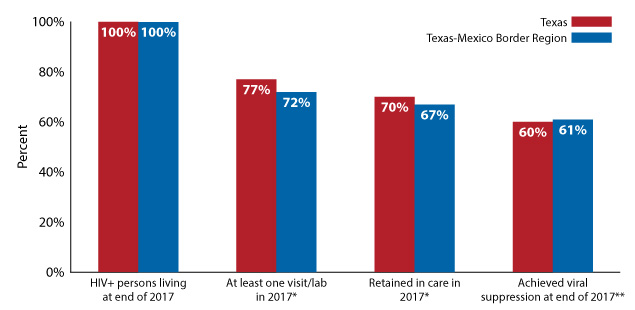
Source: Texas eHARS as of July 13, 2018
* DSHS HIV Unmet Need Project, 2017 (incl. eHARS, ELR, ARIES, ADAP, Medicaid, private payer data).
** Electronic Lab Records, ARIES labs, ADAP labs, 2017
Data for Figure 5
HIV, STDs, and TB in the Texas-Mexico Border Region